At this time in the US, Regenerative Medicine (orthobiologics) is based on Platelet Rich Plasma (PRP), Bone Marrow Aspirate Concentrate (BMAC), and Microfragmented Fat (MFAT) as overseen by the FDA. All three are point-of-care approaches, meaning office-based procedures. By the same token, none are indemnified by third parties, i.e. covered by insurers.
If we review the emerging discipline of Regenerative Medicine, there are two general categories:
1) Symptom reduction
2) Regeneration
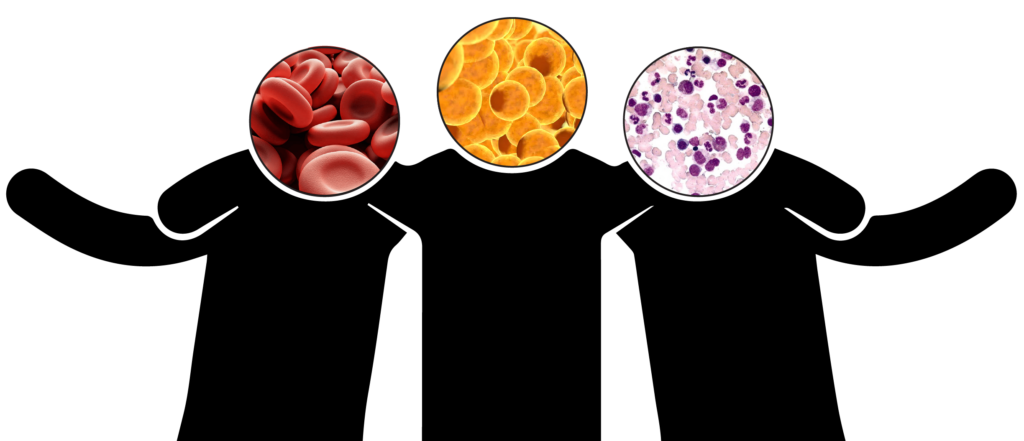
PRP in Regenerative Medicine
PRP obtained by venipuncture and centrifugation addresses symptoms only. When activated, proteins called growth factors contained therein may help reduce the inflammation associated with osteoarthritis and tendinitis, thereby reducing pain and improving function. PRP is not regenerative because it contains no stem cells; it is only anti-inflammatory, a symptom-reducing pain reliever. BMAC and MFAT with their inherent stem cells are regenerative as well as symptom reducing, so they have long term implications of healing; PRP has a comparably short timeline of symptom relief and little assistance in repair.
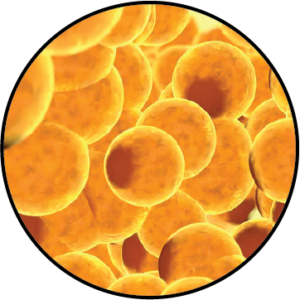
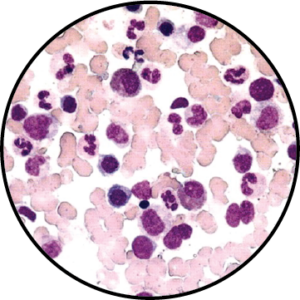
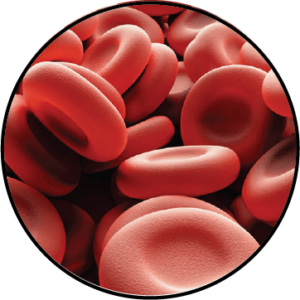
MFAT and BMAC in Regenerative Medicine
MFAT is a form of processed adipose tissue that has been broken down into small fragments or particles. Because the MFAT contains abundant stem cells, it is regenerative in nature. BMAC, a mixture of white blood cells, platelets, growth factors, and proteins, also contains stem cells and is regenerative.
Medical science is presently unable to conclusively determine the superiority of MFAT vs. BMAC in patients under age 60. We need more research. We at Jointechlabs, in a joint venture with Apex Biologix, are conducting clinical research in this area. However, BMAC contains far fewer mesenchymal stem cells (MSCs), the cells primarily responsible for regeneration, relative to MFAT. In fact, BMAC contains 0.001% MSC vs 1-10% in MFAT, and as we age the number of stem cells contained in BMAC further diminish so after age 60, MFAT is a better option for regeneration. Stem cells in fat do not diminish with age and remain vibrant through life, so it’s likely that medical research will show that MFAT is the superior regenerative agent at any age.
At present, it is for the clinician to recommend whether a patient’s regenerative needs are best served by the stem cells in bone marrow, recognizing there are far fewer compared to MFAT, where there are a significantly greater number of stem cells available for regeneration.
Additionally, for patients with a history of cancer, radiation, bone marrow diseases, and certain co-morbidities, or for those dependent on specific pharmacologics, BMAC is not an acceptable option, while MFAT may be and MFAT also has cushioning properties.
MFAT has fewer contraindications for use as the adipocytes or fat cells protect the stem cells in the fat. Additionally, the aspiration (extraction) process for adipose tissue (MFAT’s precursor) is much less painful for the patient than the aspiration process for bone marrow.
PRP Together With MFAT
As stated above, PRP is a very effective anti-inflammatory. Yet when combined with MFAT, there is a more immediate reduction of symptoms than when applied alone. Additionally, there is the regenerative benefit of stem cells contained in the MFAT delivered to the patient.
Summary
All three – PRP, BMAC and MFAT – are autologous, i.e. derived from you and not donated. PRP is anti-inflammatory with little if any regenerative potential. BMAC becomes less effective as we age and even earlier in life has comparatively few stem cells compared to MFAT. MFAT has fewer contraindications and abundant stem cells for regeneration.
I predict as clinicians become as familiar with mini liposuction as they are with bone marrow aspiration, we will see an exponential increase in the application of MFAT to reduce the symptoms and reverse the limited function imposed by osteoarthritis.